Clinicopathological markers associated with recurrence in ductal carcinoma in situ of breast by age group
Article information
Abstract
Purpose
In the present study, factors related to the recurrence of breast ductal carcinoma in situ (DCIS) in Korean patients were identified, and the prognostic factors for each age group were explored.
Methods
The subjects were 226 patients who were diagnosed with DCIS by histopathologic examination, and the effect of representative prognostic factors that are known already, including estrogen receptor (ER), progesterone receptor (PR) and the human epidermal growth factor receptor 2 (HER2) status, Ki-67 levels, and adjuvant therapy on the recurrence of DCIS was analyzed by using the Cox proportional hazard model.
Results
Among the 226 subjects, 11 patients underwent the recurrence of breast cancer. The average follow-up period was 52.7±23.5 months. The average age of the subjects was 50.6±9.3 years. Among the DCIS patients, the recurrence of breast cancer was significantly higher in the ER negative patients and those who have a Ki-67 level over 20%. However, the PR and HER2 status did not significantly affect breast cancer recurrence. The result also showed that only ER negative was a significant factor before the age of 50 years and that only the Ki-67 level over 20% was a significant factor to the patients 50 years of age or older.
Conclusion
DCIS patients should be appropriately treated and managed depending on their age and clinicopathological factors to prevent the recurrence of DCIS.
INTRODUCTION
Breast cancer is the cancer showing the second highest early incidence rate among Korean women (75.1 cases out of 100,000 women, 2015), following thyroid cancer [1]. The incidence rate of breast cancer is ranked fifth in the entire population including men and women and increased by 16.6% in comparison with 2005, and the number of deaths and the mortality are also increasing continuously [2]. In addition, according to a report published by the Korean Breast Cancer Society in 2006 [3], about 20% to 30% of breast cancer patients have experienced a recurrence, and about 71% of the patients who had already undergone a surgery after a recurrence have experienced a second recurrence within 3 years.
Ductal carcinoma in situ (DCIS), a noninvasive cancer, has rapidly increased with the recent advancement in the breast cancer diagnosis. According to a study recently conducted in the United States, DCIS accounts for about 25% of total breast cancer incidents [4–6]. The incidence rate of DCIS in Korea is also increasing steadily [7].
The prognostic factors of breast cancer that are conventionally known include the tumor size, lymph node metastasis, estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2) status, and Ki-67 levels [8,9]. As the incidence of DCIS is significantly increasing, the prognostic factors of the DCIS have been investigated. According to a study conducted with 458 subjects in 2013, the survival rate was low in triple negative patients who were found negative in all ER, PR, and HER2 [10]. Williams et al. [11] reported in 2015 that the recurrence rate of all subtypes of invasive cancers, except the luminal A type with positive ER and PR and negative HER2, was increased as the Ki-67 level was increased.
In Korea, few studies have been conducted on the prognostic factors of DCIS. The study conducted with 381 DCIS patients in 2010 showed that the local recurrence rate was higher in young, and ER positive patients who have not undergone tamoxifen treatment [12]. The present study was conducted to identify the factors related to the recurrence of DCIS and to explore the prognostic factors for each age group.
METHODS
Study population
The subjects of the present study were 226 patients who were finally diagnosed with DCIS by histopathologic examination at the Department of Surgery in Gachon University Gil Medical Center from January 2007 to December 2015. The information about the patients’ age at the diagnosis, family history of breast cancer, menopausal status, the number of childbirth, surgical method, the ER, PR and HER2 status, Ki-67 levels, adjuvant chemotherapy, adjuvant hormone therapy, and adjuvant radiotherapy were collected from their medical records.
Statistical methods
The final endpoint was defined as the recurrence of breast carcinoma in situ or invasive breast cancer following the diagnosis of breast DCIS. The time variable in the patient with recurrence was defined as the period from the date of diagnosis until the confirmed date for recurrence. The breast cancer patients who did not have the confirmed evidence on recurrence were censored at the date of final observation. A log-rank test was performed to compare the recurrence considering with the period to the recurrence according to basic characteristics, including the age at diagnosis categorized by the age of 50 when menopausal usually occurs, family history of breast cancer, menopausal, the number of childbirth (less than two times or two times or more), surgical method, and adjuvant therapy. In addition, an age-adjusted Cox proportional hazard model was used to analyze the effect of prognostic factors of breast cancer, including ER and PR, which are the known prognostic factors, as well as the hormone receptor status where only those who are found negative in both the ER and PR levels are defined as negative, the HER2 status and a prior defined categories of Ki-67 level [13]. To explore the age-specific prognostic factors, the subjects were stratified by the age of 50 years for the analysis. All the analyses were performed by using SPSS. The P-value less than 0.05 was defined as a level of significance.
The present study was approved by the Institutional Review Board of the Gil Medical Center (IRB No. GAIRB2018-178). The informed consent was waived.
RESULTS
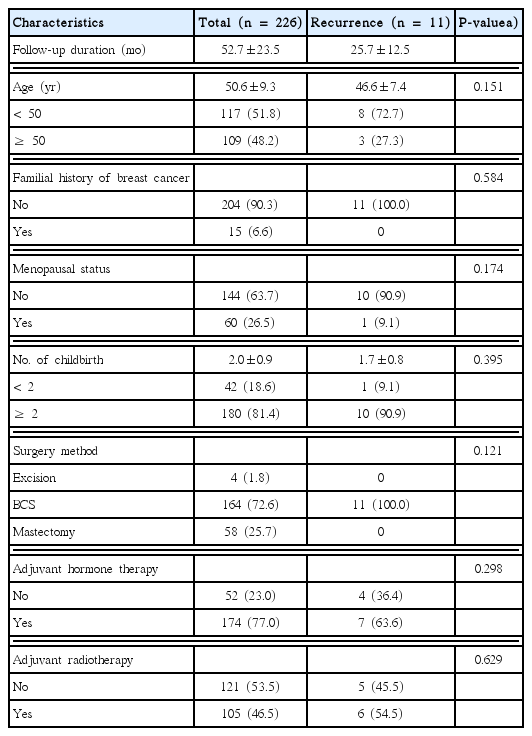
Table 1 shows the recurrence according to basic characteristics of the subjects. Among the 226 subjects, 11 patients underwent the recurrence of breast cancer. The average follow-up period was 52.7 ± 23.5 months. The average age of the subjects was 50.6± 9.3 years. The average age of the subjects at recurrence was 46.6± 7.4 years. The age groups categorized by the age of 50 years showed no difference in the recurrence and the recurrence period. The family history of breast cancer, menopausal, number of times of childbirth categorized by two times of childbirth, surgical method, and adjuvant therapy show no difference in the recurrence and the recurrence period, either.
Table 2 presents the status of clinicopathological characteristics for the 11 patients of recurrence group. Five of patients recurred with DCIS and three with invasive ductal carcinoma (IDC), and there were also one of lobular carcinoma in situ, invasive lobular carcinoma, and Paget’s disease, respectively. Seven of patients recurred in the same site and four of patients recurred in the contralateral breast. In the recurrence group, ER and PR were negative in six patients, and hormone receptor status was negative in five patients, and HER2 status was negative in four patients. The Ki-67 level was found to be more than 20% in five, more than 10% in two, and less than 10% in four patients.
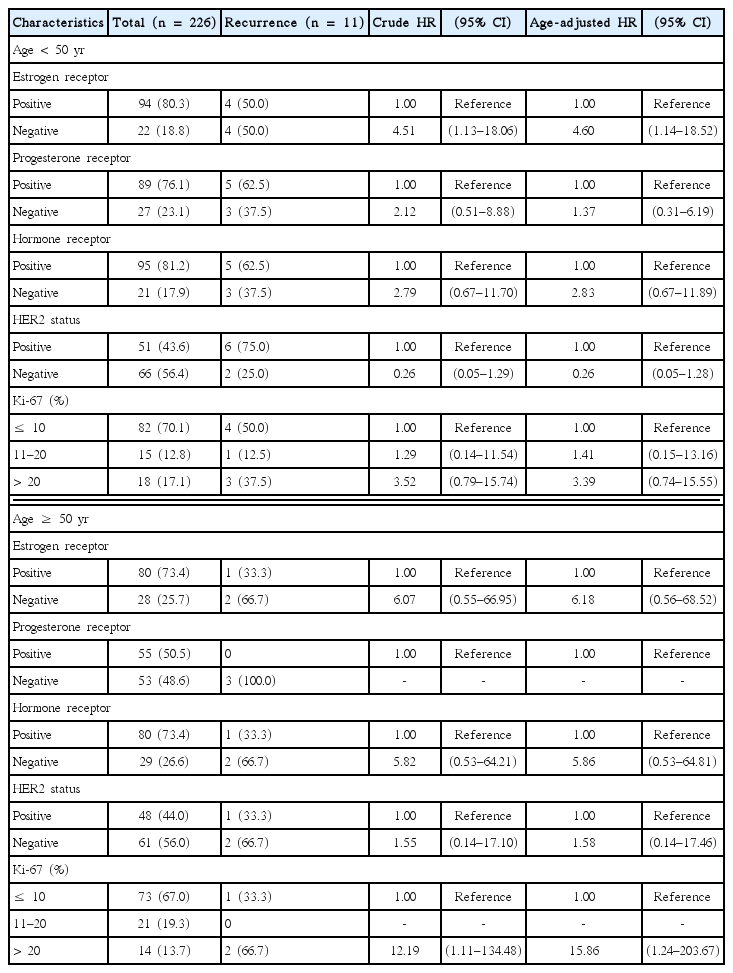
Table 3 shows the association of the ER, PR, hormone receptors and HER2 status, and Ki-67 level with the recurrence in the total DCIS patients. The breast cancer recurrence rate was significantly higher in the ER negative patients or the patients with a Ki-67 level over 20%. The significance was preserved also in the age-adjusted Cox proportional hazard model. In contrast to the ER status and the Ki-67 level, the PR and HER2 status did not show a significant effect on the breast cancer recurrence. However, the age-adjusted analysis suggested that the hormone receptor status may increase the risk of breast cancer recurrence.

Associations of hormone receptors status, HER2 status, and Ki-67 level with recurrence of breast cancer in 226 DCIS patients
In Table 4 stratifying all the subjects by the age of 50 years, only the ER status showed a significant effect on the recurrence in the patients younger than 50 years. In the patients 50 years or older, only the Ki-67 level over 20% significantly increased the risk of recurrence.
DISCUSSION
Through the follow-up survey for an average period of 4.3 years, we found that different clinicopathological factors affect the recurrence of breast cancer of different age groups. A total of 11 breast cancer recurrences were found during the follow-up. The factor that showed a significant association with the breast cancer recurrence was the ER status in the patients before the age of 50 years and the Ki-67 level in the patients aged 50 years or older.
DCIS is known as non-obligate precursor of invasive breast cancer, and less than 40% of DCIS is progressed to the invasive disease when patients had not been treated [14]. Until recently, the precise mechanism of the major driver acting on the development of DCIS into invasive breast cancer has not been elucidated. However, previous studies have reported that DCSI and IDC are remarkably similar, and that a series of processes occurs through genetic, epigenetic aberrations in some subsets of DCIS cells and molecular mechanisms associated with micro-environmental factors [15–18].
Clinicopathological factors revealed in the present study were consistently identified in the previous study. In ER, PR, and HER2 status, Roka et al. [19] reported that the recurrence rate was significantly higher in the ER negative patient group than in the ER positive patient group. Kerlikowske et al. [13] conducted a study with 324 DCIS patients and reported that the ER negative status was not significantly associated with the recurrence as an invasive cancer but significantly increased the recurrence risk of DCIS. They also reported that the recurrence risk of DCIS was even higher in the ER negative, HER2 positive and high level of Ki-67. The effect of the Ki-67 level investigated in the present study was also similar to the results found in previous reports. Chasle et al. [20] reported that the global proliferation factor indicated the level of Ki-67 and cyclin is a predictor of the recurrence of the breast cancer. Barnes et al. [21] reported that the recurrence rate was increased as the Ki-67 level was increased.
The result of the present study additionally suggests that different factors may be involved in the recurrence in different age groups. Previous studies have shown that the recurrence rate was higher in younger age groups, especially higher in the age group below 49 years than in the age group over 50 years [22], or the recurrence rate was higher more than two times in the patients at the age of 40 years or younger [23]. A study conducted in Korea also showed that the recurrence rate was higher in younger patients [12]. Although there were suggestions that the reason for the higher recurrence rate in younger patients may be the lower hormone receptor expression level, which is consistent with our study, an association between the hormone receptor expression level and age group was not found. Further study will be needed to reveal the mechanism of how hormonal receptors are acting in the progression of DCIS.
When interpreting the result of the present study, it should be considered that the number of patients who underwent the DCIS recurrence was extremely small. Thus, we could not divide the recurrence group into invasive and noninvasive breast cancer. However, the recurrence, metastasis, and mortality of the DCIS are known as very low [6]. Therefore, most of the previous studies were also conducted by using the local recurrence, including both invasive and noninvasive breast cancer as an outcome. In addition, the statistical power to capture precise effect of clinicopathological factors on the recurrence of DCIS may be insufficient. However, the present study has the strength of being able to propose the possibility of different prognostic factors of DCIS depending on the age group for the first time. Moreover, in present study, we could not consider the subtype of DCIS. The effect of clinicopathological factors on the prognosis of breast cancer according to subtype of breast cancer should be evaluated in the further study.
The present study showed that the ER status and the Ki-67 level affect the recurrence in breast DCIS patients, indicating that the prognostic factor is the ER status before the age of 50 years and the Ki-67 level after the age of 50 years. Therefore, the DCIS patients should be treated and managed depending on the age and the clinicopathological marker status to prevent the recurrence in the patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.