ABSTRACTPurposeThe incidence of poorly differentiated thyroid carcinoma (PDTC) is extremely low among thyroid cancers and there is no standardized treatment guideline for it. In this study, we have analyzed PDTC patients and reviewed their clinicopathological features.
MethodsData of PDTC patients from our institution are collected through the electronic medical database. We analyzed them by several parameters such as basic demographics, presenting symptom, preoperative cytology results, associated pathology, surgical results, surgery type, and distant metastasis.
ResultsWe collected 23 cases in our institution. Apart from two patients who were transferred to another hospital upon diagnosis, all 21 operated cases are analyzed. The parameters we studied were age, sex, presenting symptoms, distant metastasis and pathological features such as tumor size, associated pathology, predominant pattern and so on. We also provided descriptive analyses according to the type of presentation and treatment; patients with distant metastasis, juvenile cancer, and concurrent hyperthyroidism. Furthermore, we provided different cases in which the initial surgical plans differed.
INTRODUCTIONPoorly differentiated thyroid carcinoma (PDTC) is an intermediate entity on the spectrum between well-differentiated and anaplastic carcinoma and may represent a transitional form, with a reported incidence from 2% to 15% of all thyroid cancers [1–3]. The variation in incidence may reflect geographic influences or differences in histopathological interpretation [4].
PDTC represents the main cause of morbidity and mortality from non-anaplastic follicular cell-derived thyroid cancer and is therefore clinically highly significant. Nonetheless, studies on PDTC have been limited due to its relative rarity and heterogeneity of inclusion criteria [5].
Because of the small number of patients diagnosed with PDTC, there is little consensus on the optimal treatment approach for newly diagnosed patients or in which combination the treatment modalities should be offered. In this light, the present study’s aim was to provide the experience of a tertiary medical center with PDTC within a 5-year period evidence to add to the existing literature by. We reported 23 cases of PDTC with their clinicopathological features, extracted typical cases and reviewed and compared them with the previous medical literature.
METHODSWe reviewed all cases of PDTCs diagnosed and archived in the electronic medical database from 2015 to 2020 at Gachon University Gil Medical Center. The clinical, follow-up and previous fine-needle aspiration cytology (FNAC) information were obtained from the medical records of the patients. FNAC smears, hematoxylin and eosin stained tissue sections and their immunohistochemical stained slides of all cases were reviewed. The parameter collected were tumor size, associated histopathology, predominant architectural pattern, presence/absence of convoluted nuclei, tumor necrosis, mitotic count, lymph node involvement, vascular invasion, distant metastasis, and outcome of patient. Descriptive analysis was done on the data because of there were no morbidities or mortalities related to the cancer, and the number of cases were too small. A portion of the representative cases were described. Institution review board approval (IRB No. GBIRB2020-183) was acquired for retrospective analysis.
RESULTSClinicopathologic characteristicsDuring the study period, 23 patients were diagnosed with PTDC. The mean age at diagnosis was 52.0±19.1 years, seven patients (30.4%) were male and 16 (69.6%) were female. Twelve patients (52.2%) were younger and 11 (47.8%) were older than 55 years of age. Among the 23 patients, two received operations at another institution upon being diagnosed with PDTC. Among the 21 PDTC patients operated in our institution, 11 (52.4%) were incidentally discovered, eight (38.2%) presented with growing neck mass and one (4.7%) presented with acute dyspnea at the emergency department and another patient (4.7%) with swallowing discomfort. Only eight patients (38.1%) received initial total thyroidectomy and subsequent radioactive iodine (RAI); three patients (37.5%) changed plans from lobectomy to total thyroidectomy because intraoperative frozen section revealed cancer, two patients (25%) had preoperative diagnosis of distant metastasis, there was a patient (12.5%) with compressive symptom, with concomitant hyperthyroidism, and with an indeterminate contralateral nodule each. Among the other 13 patients (61.9%), 10 (76.9%) received completion thyroidectomy and subsequent RAI whereas the remaining three (23.1%) did not receive further treatment and are closely monitored. All 21 patients (100%) operated cases were reported to be minimally invasive PDTC with no case of widely invasive cases. The predominant pattern was not reported in 12 cases (57.1%), trabecular in six cases (28.6%) and insular in three (14.3%). There was no locoregional lymph node metastasis nor convoluted nuclei in any patients. Necrosis was discovered in three of the nine reported cases (33.3%) and vascular invasion was present in nine of all 21 cases (42.9%). A total of four patients (38.1%) suffered from distant metastasis. Metastatic lesion included two in the lung and two in the bone. All patients survived at the time of analysis and the median follow-up period was 24 months (range, 1–60 months).
Descriptive analysis of typical patients from our institutionThe descriptive analysis of the 21 patients are summarized in Table 1, while 16 cases are explained in further detail. The remaining five cases were excluded because they presented similar chief complaint, medical history and pathologic features compared to the other 16 cases.
PDTC presenting with distant metastasisCase 1A 63-year-old female patient presented to our institution with a palpable non-tender mass in the neck. Upon ultrasonography, three nodules of 2.5 to 0.9 cm in diameter were discovered. Consecutive FNAC retrieved suboptimal specimen and the patient was followed. Four years after the first visit the patient presented with a slight voice change and the diameter of the thyroid nodules slightly increased. She was followed up 4 years later after visiting a local clinic but further FNAC results were again non-diagnostic. During the next 2 years her voice change aggravated and at age 74 years, her core needle biopsy results revealed suspicious papillary thyroid carcinoma (PTC). Surgical pathology results, upon receiving total thyroidectomy, revealed a 5.5 cm PDTC with trabecular and solid pattern (90%). Subsequent RAI whole body scan (WBS) indicated iodine uptake in both lungs and the skull (Fig. 1). Despite multiple metastasis the patient refused further treatment due to poor general condition and performance status and is survived after 11 months of follow-up. Her final serum thyroglobulin (S-Tg) level was 7.6 ng/mL.
Case 2A 73-year-old female patient presented with a 6.6 cm right 1st rib mass which was incidentally found on chest computed tomography (CT) scan before an orthopedic surgery for a right shoulder fracture. Bone biopsy of the lesion revealed hyperplastic thyroid tissue suspicious of metastatic follicular carcinoma or metastatic follicular variant PTC. Surgical pathology report following a total thyroidectomy revealed a 0.8 cm and 0.4 cm PDTC with concomitant 0.7 cm PTC and 0.3 cm minimally invasive follicular thyroid carcinoma (FTC) in the left thyroid gland. She received high dose RAI treatment 2 months after surgery. The WBS results indicated multiple bone metastasis in the skull, ribs, spine and pelvis. On postoperative 1-year follow-up chest CT, the initial metastatic bone mass decreased in size to about 5.5 cm while other bone lesions remained similar in size. Her S-Tg level remained above 250 ng/mL ever since the surgery. She is survived 12 months after operation despite the persistent metastatic lesions.
Case 3A 73-year-old male patient presented with a sudden swallowing discomfort. Ultrasonography revealed a 6 cm nodule in the left thyroid of which the FNAC results were non-diagnostic. Left thyroidectomy was performed due to the symptom. Surgical pathology report revealed insular PDTC with squamous differentiation. He received completion thyroidectomy 4 months later and received high dose RAI which at the time did not reveal evidence of distant metastasis. Follow-up chest CT done 4 years later revealed lung nodules consistent with pulmonary metastasis despite normal S-Tg levels. However, patient refused further treatment and is survived after 46 months of follow-up.
Case 4A 38-year-old female presented to the clinic with a cervical mass that had been growing for the last 2 years. She also had compressive symptoms in supine position. Subsequent FNAC and revealed follicular lesion of undetermined significance on right thyroid lobe. After receiving right thyroid lobectomy, the surgical pathology report revealed 5.7 cm PDTC (70%) with insular and solid pattern, arising in follicular carcinoma (Fig. 2). A completion thyroidectomy and high dose RAI were performed 1 month. The WBS reported hazy uptake on the mediastinum and both lung fields indicating possible pulmonary metastasis. Subsequent chest CT, positron emission tomography (PET), and bone scan results indicated atypical adenomatous hyperplasia of the lung, focal mild hypermetabolic lesions in the upper inner left breast respectively, and no bone scan abnormalities. She is being closely monitored for possible progression of lung lesions while her final S-Tg level remained low at 0.43 ng/mL 9 months after the surgery.
Juvenile PDTCCase 5A 15-year-old female patient presented to our institution with a 2.4 cm hypoechoic lesion in the right thyroid lobe which was incidentally discovered during work-up for a medical condition un-related to thyroid. Subsequent FNAC result indicated suspicious PTC and the patient was admitted for planed right thyroid lobectomy until intraoperative frozen section results indicated PTC versus PDTC after the operation was extended to total resection of both thyroid glands. Surgical pathology report revealed a 2.4 cm PDTC arising amidst PTC on right thyroid lobe. She received high dose RAI 2 months after surgery which did not reveal any metastatic lesions. While she had clinical follow-up at intervals of about 6 months, mild increased uptake in the left femoral neck on WBS was appeared 3 years after surgery. However, the femur X-ray showed the lesion was more likely bone island. Her final S-Tg level was 0.73 ng/mL at 58 months after the surgery without further evidence of recurrence.
PDTC with concurrent hyperthyroidismCase 6A 64-year-old male patient presented with severe weakness. He was diagnosed with Graves’ disease 20 years ago for which he had been on medication and under routine surveillance. Although he knew about an incidentally discovered 1 cm thyroid nodule since many years ago, no further work-up was done up to that point. FNAC report verified a 1.3 cm follicular neoplasm. A total thyroidectomy was planned for the 1.3 cm follicular neoplasm due to the concomitant hyperthyroidism. Surgical pathology report revealed 1.3 cm PDTC in left thyroid lobe and 0.2 cm PTC in right thyroid lobe. He is scheduled to receive high dose RAI.
Total thyroidectomy due to large goiterCase 7A 78-year-old female presented to the emergency department with acute dyspnea and aspiration. The patient had an emergency treatment including an intubation and presented to the intensive care unit on our institution. On the chest CT, the thyroid mass sized as 9×4.5×2.7 cm compressed the trachea, which she did not previously know of due to her large body habitus. A total thyroidectomy was performed due to huge goiter. Surgical pathologic report revealed 9.4 cm PDTC (60%) with trabecular and solid pattern in follicular carcinoma. A few days after the surgery, her respiration function was recovered and high dose RAI was performed as scheduled. No evidence of metastasis was found and her final S-Tg level was 0.44 ng/mL at 22 months after the surgery.
Total thyroidectomy due to contralateral noduleCase 8A 48-year-old female patient presented to our institution with a palpable neck mass that seemed to be growing during the previous 2 years. Ultrasonography revealed a left 4.1 cm sized oval hypoechoic mass, which was reported to be follicular neoplasm on subsequent FNAC, and a 0.5 cm ill-defined hypoechoic nodule on right thyroid lobe. Therefore, a total thyroidectomy was performed and surgical pathology report revealed a 2.2 cm PDTC, 0.8 cm PTC and 0.6 cm follicular adenoma on left thyroid lobe and a nodular hyperplasia for the right lesion. Postoperative high dose RAI did not reveal evidence of metastasis but several non-specific tiny nodules in the right lung on follow-up chest CT 6 months later were found. Short-term close monitoring and chest CT evaluation have demonstrated they have not grown or changed in size. The final S-Tg level was 0.53 ng/mL at 27 months after the surgery.
Total thyroidectomy due to cancer diagnosis in frozen sectionCase 9A 34-year-old female presented with a growing cervical mass. Ultrasonography and FNAC revealed a 4.9 cm sized mass that turned out to be suspicious for follicular neoplasm in the right thyroid lobe. Although we initially planned a right thyroid lobectomy, the plan was changed to total thyroidectomy after intraoperative frozen section verified possibility of follicular carcinoma or insular carcinoma. Surgical pathology report revealed 4.7 cm PDTC. She underwent high dose RAI and WBS did not show evidence of recurrence or metastasis. Her final S-Tg level was 0.45 ng/mL at 16 months after the surgery.
Completion thyroidectomy despite partial PTDC componentCase 10A 38-year-old male patient presented with a 2.2 cm hypoechoic right thyroid gland lesion which was incidentally discovered on carotid sonography during left shoulder pain treatment. The FNAC result on the lesion indicated follicular lesion of undetermined significance and right thyroid lobectomy was undertaken immediately. The surgical pathology report revealed a 1.3 cm PDTC (20%) with solid and trabecular pattern arising in follicular carcinoma on right lobe. After subsequent completion thyroidectomy in which there were no further lesions, high dose RAI was performed and the results indicated no distant metastatic lesions. His final S-Tg level checked 0.44 ng/mL 24 months after the surgery without evidence of recurrence or metastasis.
Case 11A 29-year-old male presented with a 5 cm sized cervical mass and swallowing discomfort. He already had FNAC report which revealed atypia of undetermined significance, favoring towards follicular adenoma. During operation, intraoperative frozen section result reported follicular neoplasm hence right thyroid lobectomy was performed. Surgical pathology report, however, revealed a 5.8 cm PDTC with trabecular pattern (20%) and a 1.3 cm PDTC with trabecular pattern (60%) both arising in minimally invasive follicular carcinoma. He received completion thyroidectomy after which the surgical pathology report revealed an additional 1 cm minimally invasive follicular carcinoma on left thyroid lobe. High dose RAI was administered and WBS did not reveal any abnormal uptake. Although chest CT follow-up 6 months later revealed subcentimeter sized nodular ground glass opacity nodules in both lungs, the characteristics, no change in nodules size in subsequent CT follow-up and S-Tg level at 0.50 ng/mL 32 months after surgery indicated no evidence or recurrence or metastasis.
Case 12A 56-year-old male, during the postoperative treatment for intracranial hemorrhage, was discovered with an incidental 3 cm sized mass on the right thyroid lobe on chest CT. However, FNAC results were non-diagnostic at that time. Follow-up ultrasonography 9 months later indicated a size increase to 4.4 cm for the hypoechoic mass which subsequent re-FNAC result indicated to be follicular neoplasm. A right thyroid lobectomy was performed and surgical pathology reports revealed a 4.4 cm PDTC (30=%) arising in follicular carcinoma. He received completion thyroidectomy 1 month after the 1st surgery which revealed only nodular hyperplasia on left thyroid lobe. He received high dose RAI treatment and subsequent WBS did not show evidence of distant metastasis. His final S-Tg level was 0.52 ng/mL at 23 months after the surgery.
Case 13A 38-year-old female patient presented to our institution with a FNAC pathologic report from a local clinic which indicated follicular lesion of undetermined significance on right thyroid. A right thyroid lobectomy was performed and intraoperative frozen section suggested follicular neoplasm. Surgical pathology report revealed 5 cm PDTC (30%) with insular pattern arising in follicular carcinoma and a 0.1 cm PTC. She subsequently underwent completion thyroidectomy and high dose RAI. After receiving RAI, however, she wanted to move to other hospital. Thus, we followed the patient for only 2 months during which her final S-Tg level was 0.65 ng/mL.
Thyroid lobectomy despite partial PTDC componentCase 14A 43-year-old female patient presented to our clinic with an incidentally discovered 0.6 cm nodule at the right thyroid lobe on ultrasonography which was reported to be suspicious for PTC on FNAC. A right thyroidectomy was planned to be undertaken but intraoperative frozen pathology reported a possibility of suspicious anaplastic thyroid cancer (ATC). Because the chances of ATC occurring at such young age was improbable, the surgeon did not change plans and concluded the operation with right thyroid lobectomy surgical pathology report revealed 1.2 cm PDTC (50%) associated with PTC, mixed conventional and follicular pattern amidst Hashimoto thyroiditis. No further completion thyroidectomy and hence no RAI was undertaken after the patient was fully informed of the situation. Multiple PET, bone scans, and chest CTs did not reveal evidence of recurrence or metastasis at 39 months after surgery.
Case 15A 47-year-old male patient presented to our institution with palpable mass on right neck. Ultrasonography revealed about 6.2 cm sized oval predominantly solid isoechoic mass on right thyroid lobe. Subsequent FNAC report indicated possible follicular variant PTC or follicular carcinoma. He underwent a right thyroidectomy and intraoperative frozen section reported possibility of Hurthle cell carcinoma versus oncocytic and follicular variant PTC. However, final surgical pathology report revealed a 6.5 cm PDTC (30%) associated with well-differentiated thyroid carcinoma with follicular and oncocytic feature. After the surgery, follow-up chest CT and bone scan revealed no significant abnormality. His S-Tg level was within normal range during 26 months of follow-up.
Case 16A 32-year-old female patient presented to endocrinology department with outside FNAC report indicating a 2 cm suspicious for atypical follicular nodule on left thyroid lobe. Her re-examination including ultrasonography and FNAC reported a 2.2 cm ill-defined hypoechoic mass which was suspicious for follicular variant PTC or PTC. She underwent left thyroidectomy by for which surgical pathology report revealed a 1.7 cm PDTC with trabecular pattern scattered within a PTC lesion hence the unmeasurable PDTC component percentage. Further treatment was not undertaken after acquiring patient consent. Postoperative ultrasonography and neck CT did not reveal evidence of distant metastasis. She was monitored for 20 months without recurrence after which she moved to an institution closure to her residence. Her final S-Tg level was 0.58 ng/mL.
DISCUSSIONThe treatment of PDTC has not been standardized unlike differentiated thyroid carcinomas for several reasons.
First of all, the extremely low incidence of the disease and heterogeneity of inclusion criteria, i.e., the Memorial Sloan Kettering Cancer Center-PDTC [6] and Turin-PDTC criteria [7] make it difficult to conduct large scale studies necessary in devising a standard guideline. Despite the universal agreement on the diagnosis of PDTC, pathologists differed on its histologic definition. Before 2004, PDTC was known as insular carcinoma until the World Health Organization recognized it as a separate entity. While some relied on a growth pattern (solid/trabecular) alone [8], others used high mitotic rate and/or tumor necrosis for diagnosis [6]. In 2006, an international pathologist group issued the following PDTC diagnostic criteria in Turin, Italy (Turin-PDTC): (1) solid/trabecular/insular pattern of growth; (2) absence of conventional nuclear features of PTC; and (3) at least one of the following features: convoluted nuclei, mitotic activity ≥3/10 high power microscopic fields, and tumor necrosis [7].
Moreover, PDTCs are difficult to diagnose by FNAC which is the preoperative diagnostic method of choice for thyroid nodules. Although high-grade features, such as necrosis and mitoses count, can be spotted in FNA material, other cytologic features of PDTC are difficult to verify in preoperative FNAC [9]. Therefore, a typical scenario of PDTC involves a patient receiving diagnostic thyroid lobectomy under the impression of follicular neoplasm or suspected FTC when in fact, the final pathology report actually reveals PDTC. In response, the surgeons will perform subsequent completion thyroidectomy and high dose RAI. This was the case for many PDTC patients from our institution.
Furthermore, indications and effectiveness regarding adjuvant therapy are not clear in PDTC. The RAI avidity of PDTC is variable [6], which is due to tumor heterogeneity and variable proportion of well and less well-differentiated tumor components. Therefore, the efficacy of RAI and the necessity of total thyroidectomy may be under question. The role of external beam radiation therapy (EBRT) equally controversial for PDTC. Although EBRT can be beneficial in differentiated thyroid cancer patients high at risk for locoregional recurrence, no significant improvement in survival has been reported in PDTC patients after receiving EBRT [1,10]. No patient from our series received EBRT.
According to previous articles the most frequent site of metastasis are the lung and bone which was demonstrated by our experience [5]. Distant metastasis rate of PDTCs is reported to range from 36% to 85% [1,5,11]. Four out of 21 patients (19.1%) were discovered with either pulmonary and/or bone metastasis. Although this rate is low compared to previous studies, the short follow-up period and lead-time bias could have led to underestimation of the true rate of distant metastasis of our patient group. Furthermore, distant control of PDTC is around 59% at year 5 [5] but likewise, our patient group’s short follow-up length prevented accurate estimation of the 5-year distant metastasis-free survival rate.
The majority of the already scarce PDTCs have occurred in old patients at a mean age of 60 years [6]. They occur extremely rarely in the pediatric population with existing literature limited mainly to case reports [12]. Recent studies have shed some light to the fact that pediatric PDTC may be genetically distinct from adult-onset PDTC considering the strong association with gene variations such as the DICER1 mutation and clinically aggressive behavior observed in a number of cases [13]. Our juvenile PDTC patient was 15 years old when she was diagnosed with her cancer. Fortunately, she was followed up for 58 months without evidence or recurrence or metastasis unlike other previous reported cases [13].
Previous reports have assessed the coexistence of hyperthyroidism with thyroid carcinomas and demonstrated that cancers are more often locally invasive, multifocal and metastatic in Graves’ disease comparison to autonomous thyroid nodules. Moreover, cancers with hyperthyroidism tend to show high recurrence rates and are usually larger than cancers with autonomous thyroid nodules [14,15]. Hyperthyroidism concomitant with PDTC, however, has rarely been reported. One case report [16] patient received operation and was followed up for 10 months without recurrence. Another patient was from a study of 347 Graves’ disease cohort [11] in which the patients natural course was not described. Our patient received total thyroidectomy believing the lesion to be follicular neoplasm, so the discovery of PTDC was incidental. However, there was too short of a follow-up period for his prognosis to be assessed, although he did present with an additional PTC.
The other cases described in the article are representative cases in which the non-standardization of treatment protocol have led to different operations. Because PDTC was not preoperatively diagnosed, total thyroidectomy was initially performed only when there was a specific reason; compressive symptom, contralateral nodule, and cancer diagnosis on intraoperative frozen section. In the remaining cases, the patients and the surgeons discovered that the lesion was PDTC at the first outpatient session after lobectomy. In the same setting, some chose completion thyroidectomy (PTDC proportion: 60%–30%) and subsequent RAI while others chose to follow-up (PTDC proportion: 30%–scattered) without further treatment. The association between proportion of PDTC in the cancer and patient outcome has not been elucidated but needs further investigation. An ideal cutoff proportion for which completion thyroidectomy and RAI treatment is unnecessary would be of great value.
The limitation of this study was the retrospective nature of the study. Furthermore, the small number of patients, short follow-up period, and the absence of both recurrence and mortality made it impossible to perform a meaningful analysis. However, the value of our experience should not be underestimated especially considering the rarity of this disease entity.
CONFLICT OF INTERESTCONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES1. Sanders EM Jr, LiVolsi VA, Brierley J, Shin J, Randolph GW. An evidence-based review of poorly differentiated thyroid cancer. World J Surg 2007;31:934-45.
2. Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid: a clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer 1983;52:1849-55.
3. Van der Laan BFAM, Freeman JL, Tsanq RW, Asa SL. The association of well-differentiated thyroid carcinoma with insular or anaplastic thyroid carcinoma; evidence for dedifferentiation in tumor progression. Endocr Pathol 1993;4:215-21.
4. Asioli S, Erickson LA, Righi A, Jin L, Volante M, Jenkins S, et al. Poorly differentiated carcinoma of the thyroid: validation of the Turin proposal and analysis of IMP3 expression. Mod Pathol 2010;23:1269-78.
5. Ibrahimpasic T, Ghossein R, Shah JP, Ganly I. Poorly differentiated carcinoma of the thyroid gland: current status and future prospects. Thyroid 2019;29:311-21.
6. Hiltzik D, Carlson DL, Tuttle RM, Chuai S, Ishill N, Shaha A, et al. Poorly differentiated thyroid carcinomas defined on the basis of mitosis and necrosis: a clinicopathologic study of 58 patients. Cancer 2006;106:1286-95.
7. Volante M, Collini P, Nikiforov YE, Sakamoto A, Kakudo K, Katoh R, et al. Poorly differentiated thyroid carcinoma: the Turin proposal for the use of uniform diagnostic criteria and an algorithmic diagnostic approach. Am J Surg Pathol 2007;31:1256-64.
8. Volante M, Landolfi S, Chiusa L, Palestini N, Motta M, Codegone A, et al. Poorly differentiated carcinomas of the thyroid with trabecular, insular, and solid patterns: a clinicopathologic study of 183 patients. Cancer 2004;100:950-7.
9. Saglietti C, Onenerk AM, Faquin WC, Sykiotis GP, Ziadi S, Bongiovanni M. FNA diagnosis of poorly differentiated thyroid carcinoma: a review of the recent literature. Cytopathology 2017;28:467-74.
10. Walczyk A, Kowalska A, Sygut J. The clinical course of poorly differentiated thyroid carcinoma (insular carcinoma) - own observations. Endokrynol Pol 2010;61:467-73.
11. Chao TC, Lin JD, Chen MF. Insular carcinoma: infrequent subtype of thyroid cancer with aggressive clinical course. World J Surg 2004;28:393-6.
12. Wu YL, Ting WH, Wey SL, Chen CK, Huang CY, Cheng SP, et al. Poorly differentiated thyroid carcinoma in a 9-year-old boy: case report. J Pediatr Endocrinol Metab 2011;24:783-6.
13. Chernock RD, Rivera B, Borrelli N, Hill DA, Fahiminiya S, Shah T, et al. Poorly differentiated thyroid carcinoma of childhood and adolescence: a distinct entity characterized by DICER1 mutations. Mod Pathol 2020;33:1264-74.
14. Pellegriti G, Belfiore A, Giuffrida D, Lupo L, Vigneri R. Outcome of differentiated thyroid cancer in Graves’ patients. J Clin Endocrinol Metab 1998;83:2805-9.
Fig 1Whole body scan image revealing multiple bone (yellow arrowheads head) and pulmonary metastases (red arrow). 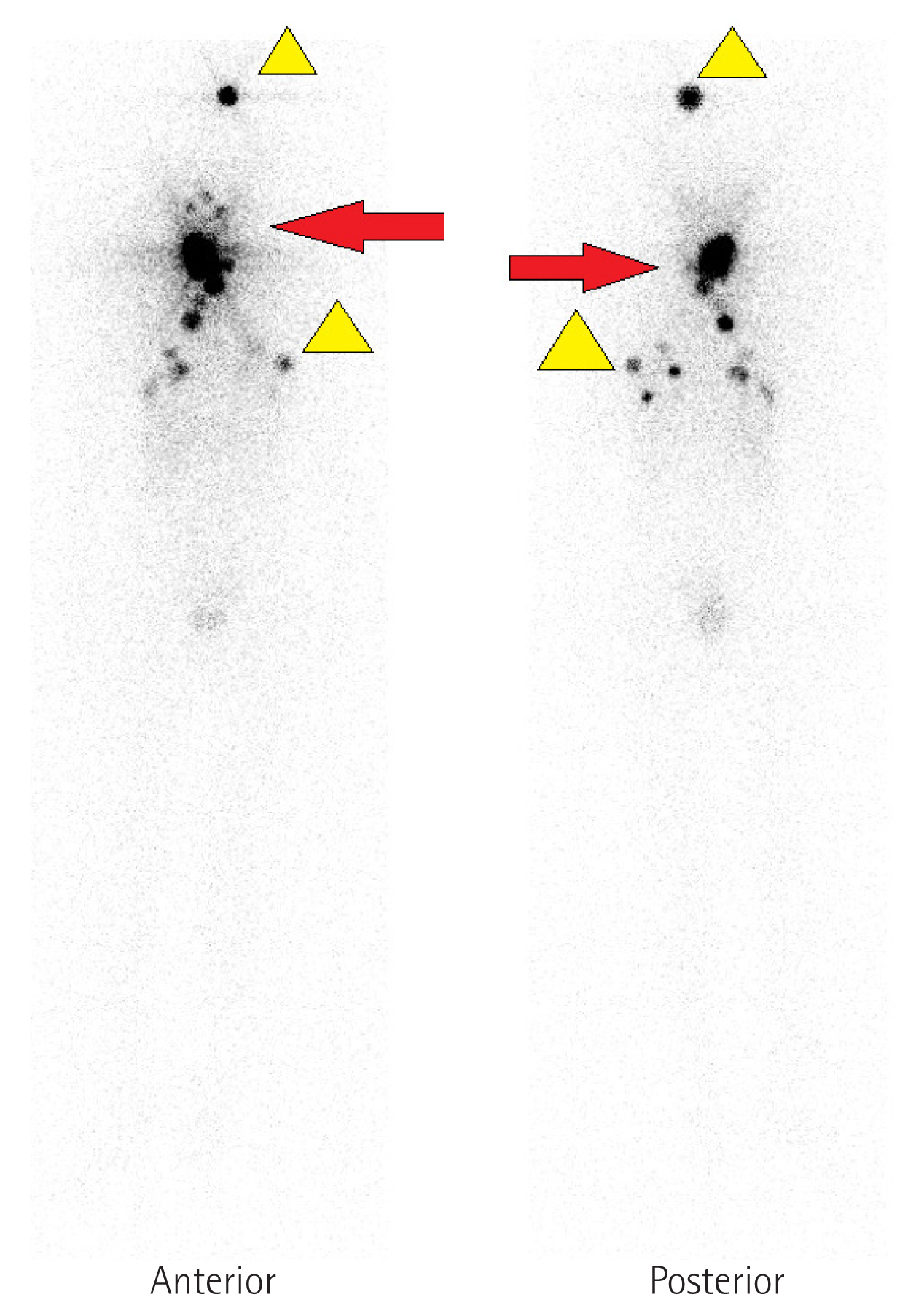
Fig. 2Poorly differentiated thyroid carcinoma slide showing insular growth pattern tumor cell nests (yellow arrowheads) separated from the surrounding stroma (H&E, ×200). 
Table 1Basic clinicopathologic characteristics FNAC, fine-needle aspiration cytology; PDTC, poorly differentiated thyroid carcinoma; HPF, high power field; F, female; M, male; FC, follicular carcinoma; PTC, papillary thyroid carcinoma; FN, follicular neoplasm; NA, non-applicable; AUS/FLUS, atypia of undetermined significance/follicular lesion of undetermined significance; FA, follicular adenoma; NH, nodular hyperplasia; HT, Hashimoto’s thyroiditis. |
|
|||||||||||||||||||||||||||||||||||